Palpitations
The most common reason for consultation in cardiology
What should you know about palpitations?
Heartbeats can sometimes feel unpleasant. This is the case when they are fast, strong, or irregular, and sometimes even when then are normal!
Caution: Resting heart rate is normal when it is between 60 and 90 beats per minute (bpm)
The causes of palpitation are always cardiac, from the mildest (the most common), to the most serious (the rarest).
What are the electrophysiological mechanisms that cause palpitations?
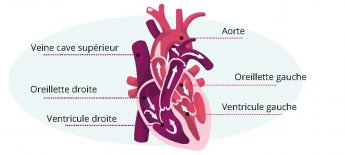
Two types of structures can be responsible for arrhythmias: either the atria (upper part of the heart) or the ventricles (lower part of the heart).
- Atrial or ventricular extrasystoles are isolated beats without any increase in the average heart rate except when they occur in bursts (but this does not last for more than a few seconds)
- Atrial or ventricular tachycardias: this is a sustained rhythm disorder with increased heart rate (usually greater than 100 bpm)
What are the symptoms of an abnormality?
The severity depends on:
- The location of the rhythm disorder (atrium or ventricle).
- Risk factors and pre-existing cardiac pathology.
- The patient's age and family medical history.
- The duration of the palpitations (isolated or persistent).
- Clinical tolerance (hemodynamics +++).
When the palpitations do occur, it is paramount to note:
- If the onset of palpitations is sudden or progressive.
- If they stop suddenly or gradually
- The duration of the symptoms (from a few seconds to several minutes or even hours)
- The tolerance (discomfort, shortness of breath, chest pain)
- The heart rate during symptoms
- the regular or irregular nature of the tachycardia
To help the doctor, the realization of an electrocardiographic at the time of symptoms is a valuable diagnostic help.
What are the risk factors for palpitations?
What are the risk factors for palpitations?
A simple physiological acceleration of the heart rate can be very badly tolerated, and you can therefore feel "palpitations": this is called "cardiac erethism". This remains a differential diagnosis, i.e. a diagnosis made when all the cardiac causes have been eliminated.
The different "pathological rhythms" causing palpitations:
Atrial stage: there is no risk of sudden death, but a stroke can occur (depending on the risk factors and the "CHA²DS²-VASC" score).
- Atrial flutter
- Atrial tachycardia
- Atrial fibrillation
Between atrium and ventricle: there is no significant risk (except if associated accessory pathway)
- Junctional or reciprocal tachycardia
Ventricular stage: Life threatening on a very short term with poor prognosis. Proven to be a life-threatening emergency
- Ventricular tachycardia
- Ventricular flutter
- Ventricular fibrillation
- Torsade de pointes
How are palpitations diagnosed at the American Hospital of Paris?
The difficulty in diagnosing palpitations lies in the fact that arrhythmias are often paroxysmal at the outset: precisely determining the rhythmical disorder at the origin of the palpitations implies being able to view it in a per-critical trace, which is not easy.
An aetiological check is urgently required, depending on the tolerance of the symptoms. A consultation with a cardiologist specialized in rhythmology (rhythmologist) with an electrocardiogram ideally during the emergency is usually the first step. The purpose of this consultation is to define the type and mechanism of arrhythmia, and to find the cause or contributing factors.
The complementary medical check generally combines:
- A biological and especially hydroelectrolytic analysis
- A transthoracic echocardiogram to find a structural abnormality of the heart
- A long-term electrocardiogram of up to 15 days (rhythmic Holter)
- If necessary, the performance of an electrical exploration of the heart (electrophysiological exploration), the implantation of an Implantable Heart Monitor and a cardiac MRI can be discussed.
What are the different treatments for palpitations available at the American Hospital of Paris?
The therapeutic arsenal includes:
- Therapeutic abstention
- avoiding and/or treating risk factors:
- treating associated pathologies: hypertension, SAS, cardiac, pulmonary, thyroid, adrenal pathologies, etc.
- helping to stop substances that excite the heart (alcohol, drugs, tobacco, energy drinks, etc.)
- Medical treatment (antiarrhythmic, anticoagulant, nodal inhibitor)
- Interventional treatment (radiofrequency ablation or cryotherapy): the strategy is to eliminate the short circuits responsible for the symptoms. This is the only treatment that can cure the pathology.
It all depends on the cause of the palpitations:
Cardiac erethism: hygieno-dietetic rule +/- medical treatment (prescription of beta-blockers)
Atrial rhythm disorder: extrasystole: simple monitoring +/- antiarrhythmic treatment
Arrhythmia: Atrial rhythm disorder: antiarrhythmic treatment +/- anticoagulant according to risk factors +/- external electric shock +/- ablation
Atrioventricular rhythm disorder: Medical treatment +/- ablation
Ventricular rhythm disorder: medical treatment / - ablation / - emergency external electric shock
Retrouvez notre brochure d'information complète
Learn more
Notre unité de cardiologie
Learn more