Insertion of a pacemaker or defibrillator
When several exams indicate the need for permanent cardiac pacing
Why propose the implantation of a pacemaker?
The decision to implant a pacemaker is taken collectively with the primary physician or cardiologist.
In a normally functioning heart, a network of electric cells depolarize and then initiate and distribute electrical impulses throughout the heart, causing it to contract. This process can be likened to the “ignition” of the heart. When the heart does not function properly, it “stalls.”
Two types of conduction problems may affect the heart:
- The first involves the initiation of the electrical impulse itself. The heart becomes electrically lazy; the sinus node, where the electrical impulse originates, no longer does its job.
- The second dysfunction is when the electrical impulse is not distributed throughout the heart.
A number of factors may alter the heart’s electrical conduction system. The most common is simply aging. Over time, the heart’s conductive capacities change. This normal phenomenon does not affect everyone in the same way: one patient may experience a conductive disorder at age 60 while an older person never has any problems.
Other factors may cause or exacerbate these issues. The main “acquired” factor is a heart attack that damages the heart’s electrical system. Some prescription medications can also lead to problems with electrical conduction. If the prescription is essential to the patient’s well-being, a pacemaker may be indicated to allow the patient to continue the treatment.
More rarely, certain heart muscle diseases can harm the heart’s electrical system.
When electrical conduction issues arise, it is necessary to restore normal functioning to the heart. Based on current knowledge, it is impossible to surgically repair the heart’s original electrical system. Similarly, there are no drugs that improve a failing system over the long term. The only solution is an implant that “fixes” the dysfunction: an artificial cardiac pacemaker.
When is the implantation of a cardiac defibrillator proposed?
Primary prevention measures consist in anticipating a potentially fatal cardiac rhythm event. People with heart disease have a significantly higher risk of sudden death than the general population. The insertion of a defibrillator makes it possible to “resuscitate” the patient in the event of fatal ventricular arrhythmia.
Secondary prevention consists in actions performed once the medical team has restored the patient’s heartbeat following a sudden cardiac near-death incident. It involves treating the recurrence when it occurs.
Patients who suffer from heart failure are the category most frequently affected by fatal heart rhythm disorders and therefore the most frequent candidates for a defibrillator. More rarely, certain heart rhythm disorders caused by a genetic disease also require a defibrillator.
How is the diagnosis made?
A clear diagnosis can be made in the presence of certain symptoms, typically electrocardiographic or structural abnormalities in the heart. In this case, the attending cardiologist or primary physician recommends the insertion of a pacemaker or defibrillator.
In other cases, the patient has symptoms which do not manifest on the electrocardiogram or clinical exam. The cardiologist therefore conducts a check-up comprising various exams in order to identify structural or electrocardiographic abnormalities.
He or she might suggest wearing an EKG monitor for 24 or 48 hours, or the implantation of a loop recorder. If necessary, an electrophysiology study of the heart can be performed on an outpatient basis to accurately measure intracardiac conduction intervals.
-
How does an artificial cardiac pacemaker work?
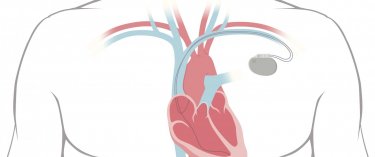
Both pacemakers and defibrillators are composed of two parts:
- The first part is the impulse generator. This hermetically sealed case made of titanium houses the pacemaker’s lithium-ion battery and software. This is the part of the pacemaker that can be felt under the skin. When the heart slows down or stops beating, one or more leads placed in the heart’s chambers measure the heart rate and relay the data to the pacemaker. In response, the pacemaker sends electrical impulses which cause the chambers to contract at a pre-programmed frequency.
- The second part is comprised of one or more leads which carry the electricity to the heart. These leads are simple electrical wires that stimulate but also monitor the heart, informing the impulse generator when cardiac stimulation is needed. It is when the lead(s) are implanted that complications may occur.
- The first part is the impulse generator. This hermetically sealed case made of titanium houses the pacemaker’s lithium-ion battery and software. This is the part of the pacemaker that can be felt under the skin. When the heart slows down or stops beating, one or more leads placed in the heart’s chambers measure the heart rate and relay the data to the pacemaker. In response, the pacemaker sends electrical impulses which cause the chambers to contract at a pre-programmed frequency.
Defibrillators have an additional function which generates a shock wave between the ventricular lead and the impulse generator in order to quickly stop a fatal ventricular rhythm event.
One of three types of pacing device will be implanted based on the number of leads implanted in the heart chambers.
The following areas can be stimulated: the upper heart (right atrium); the lower heart (left and right ventricles); the upper and lower heart. The device is chosen based on the area where stimulation is indicated.
-
What are the different types of pacing devices?
One of three types of pacing device will be implanted based on the number of leads implanted in the heart chambers.
The following areas can be stimulated:- the upper heart (right atrium);
- the lower heart (left and right ventricles);
- the upper and lower heart.
The device is chosen based on the area where stimulation is indicated.
How is a pacemaker implanted?
The implantation is a surgical procedure performed in compliance with strict asepsis protocols.
Because the surgery involves a vital organ in movement, it must be done by a cardiologist specially trained in interventional arrhythmia procedures.
Local anesthesia is sufficient, but the level of sedation may be increased if needed. An anesthesia consultation is therefore mandatory before the procedure. The pacemaker can be placed either on the right or left side, depending on the surgeon’s habits, local conditions and the individual needs of each patient.
A small incision is made under the collar bone enabling the leads to be surgically inserted through the veins to the heart. X-ray guidance is used to correctly position the leads in the heart chambers. The leads are affixed to the heart muscle and computerized tests are run during the procedure to ensure proper functioning. The patient may feel palpitations during these tests.
Once the leads have been placed, the surgeon creates a small pocket between the skin and the chest muscles where the impulse generator is inserted and connected to the leads. In thin patients, the pacemaker is visible under the skin below the collar bone. The entire procedure lasts 30 to 60 minutes, depending on the anatomical structure of each patient.
What to expect during your hospital stay
-
Admission
You will be admitted two hours before the procedure. You must stop eating and drinking by midnight the night before. You will have had your anesthesia consultation before your admission.
-
Preparing for the procedure
Your nurse will prepare you for the procedure by removing any hair from the surgical site, inserting a peripheral venous catheter and administering prophylactic antibiotics.oA patient transporter will bring you to the operating suite 30 minutes before the procedure.
-
Operating suite
You will be admitted to the operating suite by the OR nurse, who will do a final review of your medical file to ensure it is complete. You will also meet your anesthesiologist and heart rhythm specialist. The procedure can last anywhere from 45 minutes to two hours, depending on the anatomical structure of each patient and on the type of pacemaker being implanted.
-
Post-operation
After the procedure, you will be taken to the post-operative care room to ensure your safety as you wake up. Then you will be transferred to the coronary care unit for 24 hours. There you will benefit from continuous clinical observation by a cardiologist present 24/7. An echocardiogram, chest x–ray and electrocardiographic monitoring will be performed by the team.
-
Length of stay
Barring complications, your stay should not exceed 48 hours. Before you leave, all of the medical reports written during your stay will be given to you, along with your pacemaker identification card.
How to check if the pacing device is working correctly?
It is vital to regularly consult your heart rhythm specialist, who is the only person qualified to verify the impulse generator in its entirety. This is done using a computer to check all of the parameters of the pacemaker or defibrillator.
Your heart rhythm specialist ensures proper functioning not only of the pulse generator but of the heart itself in terms of rhythm. In fact, the impulse generator is equipped with an internal memory that continuously records any serious arrhythmia issues. Having this type of device is not only a useful therapeutic tool but, as is often forgotten, a valuable diagnostic tool as well. By allowing the timely treatment of arrhythmia disorders, it prevents delays that could result in serious consequences.
In recent years, telecardiology has also made it possible to perform most verification procedures remotely using a transmitter provided by the heart rhythm specialist. This considerably improves the quality of monitoring while reducing the frequency of in-person consultations.
What are the possible complications?
The implantation of a cardiac pacemaker or defibrillator is neither a complex nor a highly invasive surgery. Serious complications are rare.
However, the risks mustn’t be ignored, as some complications may have serious repercussions if tests to identify them are not systematically conducted. All risks are discussed during pre-operative visits.
You will be asked to sign an informed consent form certifying that you are aware of the risks associated with the procedure. This is by no means a liability waiver.
-
Post-operative pain
Post-operative pain is rare or very mild. Analgesics are systematically prescribed after the procedure.
-
a pacemaker changing position
- If a pacemaker lead changes position, this usually occurs in the first few days following the operation. That is why the patient is asked not to sit up until the day after the procedure. The diagnosis is made through clinical, electrocardiographic and x-ray observation. Repositioning a lead is a simple, fast and painless procedure, but requires returning to the operating room.
-
Developing a hematoma
The risk of developing a hematoma at the pacemaker site increases if the patient is taking effective antiplatelet or anticoagulant therapy. When possible, these treatments can be temporarily discontinued or reduced. A compression bandage is systematically placed after the procedure. In rare cases, the hematoma must be surgically drained if the patient is experiencing pain or if too much pressure builds under the sutures.
-
Pericardial effusion
The most serious complication is pericardial effusion, when blood builds up in the space between the myocardium (heart muscle) and the pericardium, which is a thin sac surrounding the heart. An additional and even more serious possible complication is when the heart is perforated when the leads are implanted. This generally occurs in the atria or at the top of the right ventricle. This type of internal hemorrhage develops slowly; clinical signs may be hard to detect at first and may include shortness of breath, a heavy sensation in the chest or a general feeling of discomfort. That is why we systematically perform an echocardiogram following the operation. Like any hemorrhagic syndrome, this complication is exacerbated if the patient takes anticoagulants. Treatment usually consists in performing a percutaneous puncture in order to evacuate the effusion of blood. Treating the effusion with surgery is extremely rare.
-
Post-operative rhythm disorders,
Post-operative rhythm disorders, generally affecting the atria, can develop due to temporary irritation induced by a lead. These disorders are more frequent in patients who have already experienced this type of arrhythmia. A temporary increase in the patient’s anti-arrhythmia treatment will quickly restore a normal heartbeat.
-
Abnormal contractions in the stomach
Abnormal contractions in the stomach may occur when the probe stimulates the phrenic nerve, and in the pectoral muscle due to current leakage originating in the connectors. The problem can generally be solved by reprogramming the pacemaker
-
Pneumothorax
A pneumothorax (collapsed lung) occurs when the pleura is ruptured by the practitioner during the subclavian vein puncture. The space between the pleura and the lung fills with air and the lung deflates like a balloon. It no longer functions and causes shortness of breath in the patient. This condition is easily diagnosed with a post-operative chest x-ray. Draining the air by aspiration allows the lung to very quickly re-expand and return to its normal function. This does not cause any side effects.
-
Hemothorax
Hemothorax is very rare and its mechanism is similar to a pneumothorax. In hemothorax, air is replaced by blood, usually from the accidental puncture of the subclavian artery or a ruptured brachiocephalic vein.
-
Sepsis syndrome
-
Sepsis syndrome may take on several forms:
- Immediately following surgery, typical signs of sepsis should be signaled such as fever, redness or discharge from the surgical site.
- When sepsis occurs well after the operation, treatment may be delayed because the patient is no longer hospitalized. Therefore it is important to notify the primary physician or the center where the surgery was performed of any delay in the healing process. It is important not to miss the follow-up consultation one month after the surgery. In the event of an infection, an antibiotic treatment adapted to the germ is necessary and the entire implant must be removed.
-
For patients with a defibrillator, the delivery of an inappropriate electrical shock is considered to be a complication that is easily treated by re-programming the device.
Consult our cardiologists
Learn more