Abdominal Aortic Aneurysm
Definition, symptoms and treatments
What is an abdominal aortic aneurysm (AAA)?
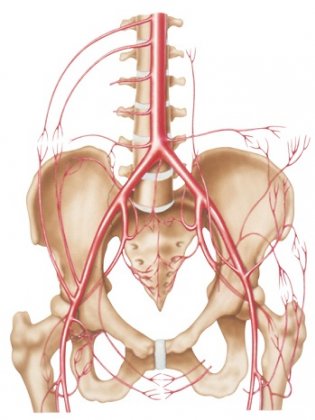
The aorta is the body’s main artery. It travels from the heart through the chest and the belly, supplying blood to all the organs, particularly those in the digestive and urinary systems.
An abdominal aortic aneurysm is a permanent, localized bulge in the part of the aorta located in the abdomen (abdominal aorta). It often occurs in the area under the kidneys, and in 80% of cases its shape is fusiform, meaning the aneurysm bulges out on all sides of the blood vessel.
Due to a person’s age or the presence of atherosclerosis, a weak spot may form in the wall of the abdominal aorta. Atherosclerosis (plaque deposits) may modify the shape of the artery walls. The aorta wall may start to swell, causing what is known as an abdominal aortic aneurysm.

As the aneurysm's diameter increases, the aorta wall grows increasingly weaker until even normal blood pressure can cause the artery to rupture, triggering severe internal bleeding.
Ruptured aneurysms are the third cause of cardiovascular disease mortality after heart attack and stroke, and were responsible for 6,358 deaths in 2008 in France, which is more than the number of deaths from road traffic accidents (source: INSERM).
What are the symptoms of an abdominal aortic aneurysm?
There are three clinical presentations:
- Asymptomatic aneurysms (majority of cases): patients have no symptoms indicating a possible abdominal aortic aneurysm.
- Symptomatic aneurysms: patients feel abdominal pain of varying intensity and location, caused when the aneurysm grows or splits.
- Ruptured aneurysms: this is a life-threatening emergency.
How is an abdominal aortic aneurysm diagnosed?
Given the absence of symptoms in most patients, aortic aneurysms are often detected during a routine medical exam, when a doctor sees or feels a pulse in the middle or lower abdomen. However, most aneurysms are discovered by chance during diagnostic imaging exams (CT scan, MRI or Doppler ultrasound) performed for other reasons.
Symptomatic aneurysms must be treated quickly as they carry a significant risk of rupturing. Because they can cause severe internal bleeding, a ruptured aneurysm requires emergency surgery.
It should be noted that 30% to 50% of smaller aortic aneurysms do not grow significantly and will not require intervention, as they present little to no risk of rupturing.
A Doppler ultrasound is the standard screening test. This non-invasive exam offers high levels of sensitivity and specificity.
Patients likely to undergo screening include:
- All men between the ages of 65 and 75, and all women in the same age group who smoke or previously smoked.
- All men and women over age 50 who have a family history of AAA
What are the risk factors for abdominal aortic aneurysm?
The risk of developing an abdominal aortic aneurysm increases with age. The condition mainly affects people 50 and over, and is more frequent in men than in women. Other risk factors include tobacco use and high blood pressure. Patients with a family history of AAA are more at risk and should discuss it with their doctor.
To prevent an abdominal aortic aneurysm, correcting certain risk factors is key, for example by giving up smoking or taking medication for hypertension.
If an aortic actasia (small dilation of the abdominal aorta) is detected during a diagnostic exam, an annual Doppler ultrasound exam will be recommended to monitor the dilated aorta. Sometimes an aortic CT angiogram is necessary.
What treatments are available for an abdominal aortic aneurysm?
Two treatment options are available for an abdominal aortic aneurysm:
1. Open repair
The surgeon makes an incision in the abdomen to access the aneurysm. A clamp is placed on either side of the aneurysm. The surgeon opens the aneurysm and removes the blood clots. The lumbar arteries that originate at the aneurysm site are sutured to prevent bleeding. Following the same principle as an arterial bypass, a synthetic tube-shaped or branched stent is then fastened to the healthy walls upstream and downstream from the aneurysm, in order to exclude the unhealthy section of the aorta and ensure blood supply to the lower limbs. The surgery is performed under general anesthesia and lasts two to three hours. Patients must generally spend one day in intensive care and remain in the hospital for at least one week. Two to three months may be necessary for a full recovery from the operation.
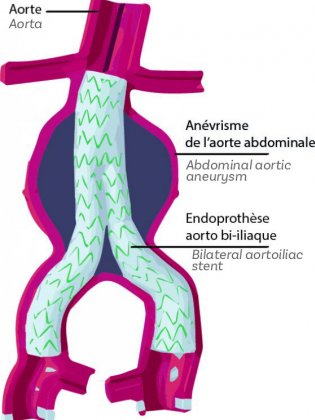
2. Endovascular aneurysm repair (EVAR)
This minimally invasive procedure is performed collaboratively by a vascular surgeon, an interventional radiologist and an anesthesiologist. It consists in placing a stent (made of metal or nitinol, a metal alloy with “shape memory” properties) covered by a leak-proof graft made of polyester fabric (Dacron) or PTFE (Teflon) inside the aorta. This technique requires no abdominal incision, and therefore leaves no abdominal scar. The stent graft is inserted through the femoral artery via an incision less than 15 millimeters long in the groin area, and delivered to the aortic aneurysm using x-ray guidance.
The operation is performed under local or general anesthesia in an angiography room or a hybrid room. It typically lasts 60 to 90 minutes, followed by a short hospital stay usually lasting three to five days. Patients do not necessarily spend any time in intensive care.
Make an appointment with our interventional radiologists
Learn moreHow does a stent graft work?
Stent grafts are designed to create a new artery wall that is hermetically sealed to prevent blood from leaking out. The goal is to alleviate the pressure on the dilated, weakened artery wall. By absorbing arterial pressure into its own walls made of Dacron or PTFE, which are both very strong, impermeable materials, the graft lowers the risk of the aorta rupturing. The stent graft is placed inside the artery walls at the aneurysm site, and the weakened artery walls are outside the stent graft. Having created a new space in which blood can flow, the stent absorbs blood pressure before it reaches the weakened artery wall.
Different stent grafts are available; the choice depends on each patient’s individual anatomy, determined through a CT angiogram performed with a contrast agent. Sometimes a stent graft is custom-made to adapt to a patient’s anatomy and the aneurysm itself.
When is it necessary to seek treatment for an abdominal aortic aneurysm?
If a doctor diagnoses an abdominal aortic aneurysm, he or she will frequently check the diameter of the aneurysm, which is the main predictive criterion for treatment. Based on how quickly the aneurysm is growing and whether it has a “saccular” shape are also decision-making factors. France’s health authority, the Haute Autorité de Santé, recommends treatment when the aneurysm diameter exceeds 5 cm for men and 4.5 cm for women, or when growth exceeds 0.5 cm in a year.

Which treatment option for an abdominal aortic aneurysm: open surgery or endovascular repair?
Stent grafts were invented approximately 35 years ago but only came into widespread use in the 1990s. They were initially used only on patients for whom surgery posed too many risks: patients with heart, respiratory or kidney failure, or having previously undergone abdominal surgery.
Today, the procedure is indicated for a much higher number of patients, provided their anatomy is suited to the operation.
The European Society of Vascular Surgery (ESVS) currently recommends stent grafting for:
- Patients with the appropriate anatomy and a reasonable life expectancy: endovascular aneurysm repair with insertion of a stent graft should be the first-line treatment (65 is considered as the reasonable threshold).
- For patients with a long life expectancy, aneurysm open repair should be the first-line treatment
The ESVS considers aortic surgery as a high-risk procedure, with a risk of death of cardiovascular origin or by myocardial infarction (heart attack) of 5% or higher in the 30 days following the operation. Mortality increases by up to 15% in patients presenting a high surgical risk due to cardiac, respiratory and renal co-morbidities. Open surgery on the aorta also has a 20% chance of causing abdominal eventration or intestinal obstruction caused by adhesions.

Institute for Health and Clinical Excellence (Institut national pour la santé et l’excellence clinique), 2020
KEY FIGURES
-
13:1 ratio
AAA occurs mainly in men, usually after age 65, with a 13:1 male to female predominance
-
Over 60
Occurrence of the disease increases with age: it affects 0.87% of the population over 60
-
High cardiovascular risk
AAA concerns approximately 4% to 6% of the male population with a high cardiovascular risk.