Embolization
What is embolization?
What is embolization?
Embolization involves injecting medications or embolic agents (designed to obstruct a vessel) through a microcatheter positioned in a vessel in order to reduce or obstruct the flow of blood in a specific part of the body.
All arteries are interconnected. This means that by injecting a product into an artery in the groin or wrist, it is possible to reach any organ and treat certain diseases without leaving a scar.
Embolization is an innovative alternative to invasive surgery. It can be performed to treat a wide range of diseases by using the body’s natural pathways or blood flow to reach an organ or pathology.
It also enables scarless outpatient procedures with very fast recovery times and an extremely low rate of complications.
How to prepare for an embolization procedure
Before the procedure, a blood test is sometimes necessary to check kidney function and the blood’s ability to clot.
The patient must inform the doctor of any medications taken, especially blood thinners, also known as anticoagulants. If the patient takes blood thinners, a “bridging” protocol using heparin is necessary, and if the patient takes several blood thinners, some of them may have to be discontinued. It is also important to signal any known allergies to Betadine, anesthesia and contrast dyes. Women must inform our staff if they are pregnant, as it is preferable to avoid exposing the fetus to the radiation emitted by the imaging machines.
If sedation or general anesthesia is used, the patient must refrain from drinking and eating six hours before the procedure. The anesthesiologist will also indicate which medications must be taken in the morning.
The patient is usually admitted one to two hours before the procedure, and discharged four hours afterward, or the next morning in certain cases.
Each medical center generally provides specific instructions on how to prepare for an embolization procedure.
What product is injected?
The embolic agent is chosen based on the disease being treated, the size of the blood vessel and whether the treatment is intended to be permanent or temporary.
Embolic agents include the following:
- Gelfoam ™, a spongy material made of gelatin that is cut into tiny pieces in order to be injected into an artery. After a period of several days to two weeks, the material dissolves.
- Microparticles, including polyvinyl alcohol (PVA) and acrylic polymer microspheres permeated with gelatin, are suspended in a liquid and injected into the bloodstream to occlude the small vessels. These agents are used to permanently block the blood vessels. The distance these microparticles will travel into the capillaries depends on their size.
- Metallic coils in a range of sizes and other mechanical devices made of stainless steel or platinum are used to block the large arteries.
- Sclerosing agents like alcohol or aethoxysklerol are used to destroy the blood vessel walls.
- Liquid glue. When injected, it hardens quickly, thereby obstructing the target vessel.
What happens during an embolization procedure?
The patient lies down on the X-ray table. An X-ray tube is positioned under the table and a detector is suspended above the table. Fluoroscopy is a technique that converts X-rays into video images. Doctors use this technique to guide their catheter to the correct position.
The patient is connected to monitors that track heart rate, blood pressure, oxygen rate and pulse.
An IV line is inserted into a vein in the hand or arm to administer a sedative. Moderate sedation is generally sufficient, without the need for intubation. However, certain patients may require general anesthesia.
The area where the catheter will be inserted is disinfected, and then a surgical field is set up.
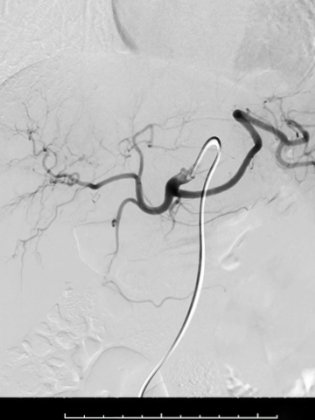
The doctor makes a very small incision in the skin. A catheter is then inserted through the incision and positioned at the treatment site thanks to image-guidance. A catheter is a long, very thin plastic tube whose diameter is smaller than a pencil lead.
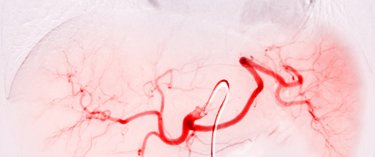
A contrast agent is injected through the catheter and a series of X-rays is taken to ensure the catheter is correctly positioned in the target vessel. The medication or embolic agent is then injected through the catheter. Additional X-ray images are taken to ensure the procedure was a success and that blood flow toward the organ or target anomaly is effectively reduced or blocked.
Once the procedure is over, the doctor removes the catheter and applies pressure to the puncture site to prevent bleeding. A closing device may be used to seal the incision in the artery. This enables the patient to move around more quickly. No stitches are visible on the skin. The nurse places a bandage over this small incision.
After the procedure, the patient must remain lying down for four hours if the groin artery was used for the procedure. If the wrist artery was used, the patient can immediately move about with a compression wristband.
The procedure can last from 30 minutes to several hours, depending on its complexity.
The IV line is removed before the patient returns home.
Who performs embolization procedures?
Embolization procedures are performed by an interventional radiologist who is specially trained in an interventional radiology surgical unit.
What conditions can be treated with embolization?
Historically, embolization was developed to stop all kinds of internal and external bleeding:
- Bleeding caused by a traumatic injury. This treatment is particularly well-suited to control bleeding in the abdomen or pelvic area due to injuries caused by a car accident.
- Bleeding of lesions in the gastrointestinal system such as ulcers and diverticular disease. Embolization is usually the first-line treatment for all types of gastrointestinal bleeding.
- Bleeding from vascular malformations and aneurisms
- Tumor bleeding
- Post-partum bleeding
More recently, embolization has been developed as an alternative to surgical techniques to treat a wide range of conditions. Blood flow plays an important role in many instances of organ dysfunction, because it supplies everything needed for a disease or symptom to develop. Modifying blood flow is the most natural way to alter the imbalances observed.
The following types of embolization have been developed:
- Tumor embolization, to reduce tumor size
- Embolization of an arteriovenous malformation (AVM) or arteriovenous fistula (AVF) (abnormal connection between an artery and a vein)
- Embolization of arterial aneurism (un bulge or “balloon” that forms in a weakened artery wall) by blocking an artery supplying the aneurism or by closing the aneurism bulge itself as an alternative to surgery
- Varicocele embolization (enlarged veins) in the scrotum that can cause infertility
- Embolization of pelvic varicose veins to block the enlarged veins in the pelvis which cause severe pain
- Prostatic artery embolization to reduce the size of the prostate gland by reducing its blood supply
- Hemorrhoidal artery embolization (HAE) to eliminate them by blocking the artery that supplies them
- Uterine fibroid embolization to reduce their size while sparing the uterus
- Embolization for frozen shoulder / osteoarthritis / tendinitis to reduce the neovessels that cause severe pain
- Embolization of congenital venous malformations (tangling of veins that have not developed into normal, straight veins) in order to reduce pain, swelling and the formation of clots
What happens after an embolization procedure?
If the procedure was performed to treat bleeding, the bleeding stops immediately after the procedure.
If the procedure involved an aneurism, thrombosis – the obstruction of blood flow – is immediate after embolization.
For embolizations of a tumor, organ, uterine fibroid or a vascular anomaly, symptoms disappear one to three months after the procedure.
What are the advantages of embolization compared to surgery?
An embolization procedure is much less invasive than conventional surgery, with a considerably lower complication rate and relatively brief hospital stay, often on an outpatient basis.
This method may be recommended to treat certain tumors or vascular malformations that cannot be removed surgically or that would involve a major risk for the patient if surgery were to be performed.
With embolization, no surgical incision is necessary. Only a tiny incision is made in the skin, and does not require stitches. Blood loss is also lower compared to traditional surgical treatments.
What are the risks of embolization?
Any procedure that involves inserting a catheter into a blood vessel carries certain risks.
After the procedure, bruises may appear, but will disappear within a few weeks. Bleeding at the puncture site may require a new compression or a minor surgical intervention to stop the bleeding. The risk of infection at the puncture site is exceptionally low.
Because a contrast agent is used during the procedure, there is a risk of allergic reaction. Allergy tests are conducted ahead of the procedure to ensure the appropriate contrast agent is used.
In patients with diabetes or a preexisting kidney disease, the contrast agent may exacerbate an already weakened kidney function. The doctor will take special measures to protect the kidney through extra patient hydration.
There is a risk, although it is quite rare, that an embolic agent used during the procedure lodges in the wrong place and deprives normal tissues of their oxygen supply. Usually, they will heal naturally within a few weeks, but additional surgery is needed in very rare cases.
After an embolization procedure, there is a risk of the target organ becoming infected, even though an antibiotic was administered. Should signs of infection appear, intravenous antibiotics are prescribed.
What are the side effects of embolization?
During the procedure, the patient does not feel the catheter inside his or her blood vessels. The only things the patient feels in the injection of local anesthesia and a slight sensation of pressure when the catheter is inserted.
During the procedure, when the contrast agent is injected into the blood vessel, this may cause a temporary sensation of heat. After the procedure, moderate pain is the most common side effect and can be managed with oral or intravenous medication.
Most patients leave the hospital within six hours after the procedure, if their pain is under control.
The patient can resume normal activities 48 hours after the procedure.
In the days following an embolization procedure, only in the case of tissular organ embolizations, a low percentage of patients develop post-embolization syndrome, whose symptoms include fever (up to 38.5°C / 101.3°F), loss of appetite, nausea and vomiting. This syndrome typically occurs when a solid tumor is embolized. The symptoms are the body’s reaction to the products that break down the tumor and occur more frequently with large tumors. They generally disappear within two to three days.
Are there any contraindications for an embolization procedure?
There are no absolute contraindications for embolization.
In the case of kidney disease or allergy to a contrast agent, the doctor must take special precautions.
Why choose the American Hospital of Paris for an embolization procedure?
Embolization is a very meticulous procedure in which the catheter must be placed in an extremely precise location to avoid damaging the normal tissues. This means the tip of the catheter must be placed in such a way as to ensure that the embolic agent is deposited only in the blood vessels supplying the area being treated. In a low percentage of situations, the procedure is technically impossible because the catheter cannot be positioned correctly. The American Hospital of Paris interventional radiology team is one of the rare teams with expertise in the direct puncture of target arteries, which considerably reduces this type of “technical failure.”
Our doctors also have expertise in the injection of all types of embolic agents, in particular liquid glue, which requires a certain dexterity and experience. This means they are able to choose the agent that is most appropriate for each patient.
